|
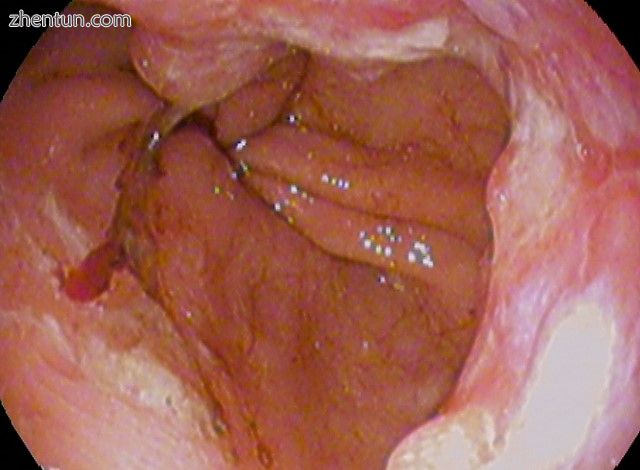
Endoscopic image of Barrett's esophagus, which is the area of red mucosa projecting like a tongue. B ...
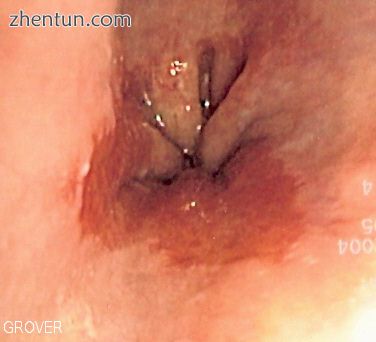
Barrett食管的内窥镜图像,是一个像舌头一样突出的红色粘膜区域。活组织检查显示肠上皮化生。
Barrett食管是指食管下部细胞的(异常)变化。其特征在于通过简单的柱状上皮替换杯状细胞的正常复层鳞状上皮衬里(通常在胃肠道中发现较低)。 Barrett食管的医学意义是它与食管腺癌(一种常常致命的癌症,[1] [2]的强关联(每1 cm布拉格C> M>每个患者年的总段长度为0.1)[1] [2]因此被认为是是一个恶化前的状况。
Barrett食管的主要原因被认为是对反流性食管炎慢性酸暴露的适应[3]近年来,西方世界食管腺癌的发病率大幅增加[1]。 5-15%的患者寻求胃灼热(胃食管反流病)的医疗护理,尽管Barrett食管患者的大部分患者没有症状[1]。
诊断需要内窥镜检查(更具体地说,食管胃十二指肠镜检查,其中通过口腔插入纤维光缆以检查食道,胃和十二指肠的过程)和活组织检查。活检后,Barrett食管的细胞分为四大类:非发育不良,低度不典型增生,高度不典型增生和明显癌。高度异型增生和腺癌的早期阶段可通过内镜切除术和新的内镜治疗如射频消融治疗,而晚期(粘膜下)通常建议接受手术治疗。通常建议非同种异体和低级别患者接受内窥镜检查的年度观察,射频消融作为治疗选择。在高度不典型增生中,患癌症的风险可能是每患者每年10%或更高。[1]
这种情况以澳大利亚胸外科医生Norman Barrett(1903-1979)的名字命名,他在1950年认为'溃疡位于鳞柱状交界处下方......代表胃内的溃疡......由疤痕组织吸入纵隔“......代表”先天性短食道“的一个例子。[4] [5]相比之下,Philip Rowland Allison和Alan Johnstone认为,这种情况与“食道内层胃粘膜,而不是Barrett错误认为的胸内胃”有关。[6] [7] Philip Allison,心胸外科医生和外科主任在牛津大学,建议“将食道的慢性消化性溃疡陨嘴称为”巴雷特溃疡“,但补充说这个名称并不意味着与”巴雷特对胃粘膜内衬胃食管的食道的描述“一致。[6] [7]
视频: ↓ 什么是巴雷特食管
https://cache.tv.qq.com/qqplayerout.swf?vid=a0755dvkng9
内容
1 症状和体征
2 病理生理学
3 诊断
3.1 筛选
3.2 肠上皮化生
3.3 上皮发育不良
4 管理
5 预后
6 流行病学
7 历史记录
8 参考
体征和症状
从正常细胞到癌前细胞的变化表明Barrett食管不会引起任何特殊症状。 然而,Barrett的食道与这些症状有关:
经常和长期的胃灼热
吞咽困难(吞咽困难)
吐血(吐血)
食道与胃接触的胸骨下疼痛
无意识的减肥因为进食是痛苦的(odynophagia)
中心性肥胖(与外周性肥胖相比)增加了发生Barrett食管的风险。[8] 确切的机制尚不清楚。 男性(更多中心)和女性(更多外周)的脂肪分布差异可以解释男性患病风险的增加[9]。
病理生理学
Micrograph of Barrett's esophagus, Alcian blue stain
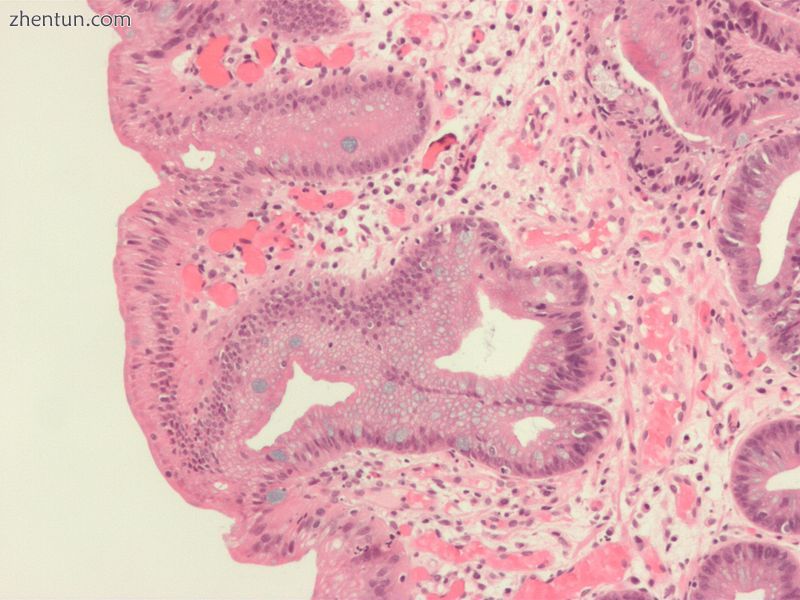
巴雷特食管的显微照片,阿尔新蓝染色
Barrett的食道由于慢性炎症而发生。慢性炎症的主要原因是胃食管反流病,GERD(英国:GORD)。在这种疾病中,酸性胃,胆汁和小肠和胰腺内容物会对食道下部细胞造成损害。最近,胆汁酸通过抑制表皮生长因子受体(EGFR)和蛋白激酶Akt显示能够在胃食管连接细胞中诱导肠分化[10]。
这导致蛋白质复合物NF-κB(NFκB1)的p50亚基最终上调,并最终激活同源盒基因CDX2,其负责肠酶如鸟苷酸环化酶2C的表达[11]。
这一机制还解释了癌症发生过程中HER2 / neu(也称为ERBB2)和过表达(谱系成瘾)癌细胞的选择,以及针对Her-2受体与曲妥珠单抗(赫赛汀)靶向治疗的疗效。治疗胃食管连接处的腺癌。
研究人员无法预测胃灼热患者会发展为Barrett食管。虽然胃灼热的严重程度与Barrett食管的发展之间没有关系,但慢性胃灼热与Barrett食管的发展之间确实存在关系。有时,患有Barrett食管的人根本没有胃灼热症状。在极少数情况下,吞咽腐蚀性物质(如碱液)可能会对食道造成损害。[需要引证]
那些患有进食障碍性贪食症的人更容易患上Barrett食管,因为贪食症会导致严重的胃酸反流,并且因为清除也会使食道充满酸性[12] [13]。
诊断
Micrograph of Barrett's esophagus (left of image) and normal stratified squamous epithelium (right o ...
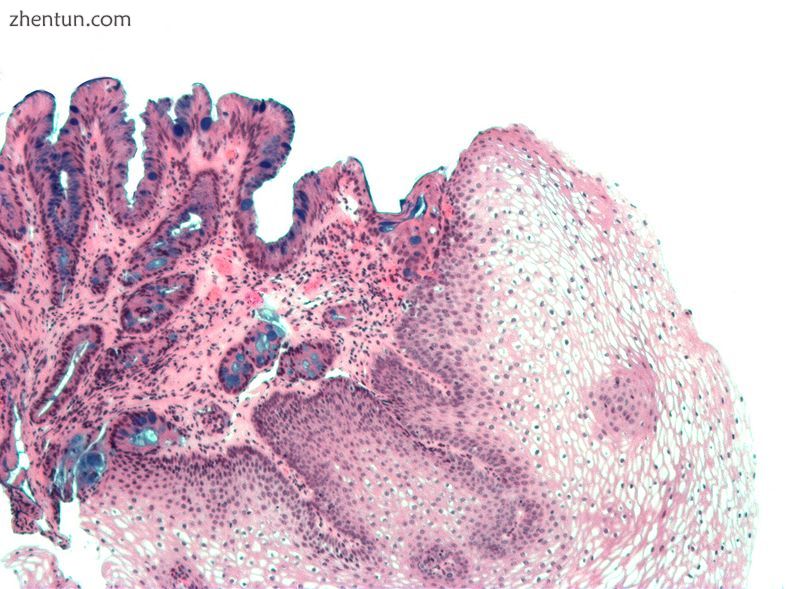
Barrett食管(图像左侧)和正常复层鳞状上皮(图像右侧)的显微照片,阿尔新蓝染色
High-magnification micrograph of Barrett's esophagus showing the characteristic goblet cells, Alcian ...
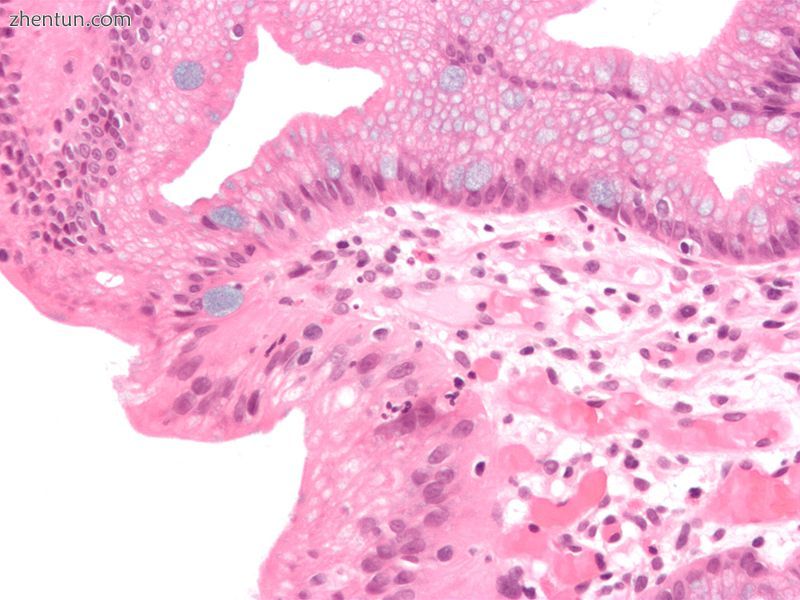
Barrett食管的高倍放大显微照片显示特征性杯状细胞,阿尔新蓝染色
需要宏观(来自内窥镜检查)和显微镜检查阳性结果才能做出诊断。 Barrett食管的特点是食管下段存在柱状上皮,取代了正常的鳞状细胞上皮 - 化生的一个例子。分泌柱状上皮可能更能够承受胃分泌物的侵蚀作用;然而,这种化生增加了腺癌的风险。[14]
筛选
建议在60岁以上的男性中进行内镜检查,这些患者的反流症状持续时间长且治疗无法控制[15]。预计不会超过5年的人不会进行筛查。[15]
肠上皮化生
杯状细胞的存在,称为肠上皮化生,是诊断Barrett食管所必需的。这经常在存在其他化生柱状细胞的情况下发生,但仅存在杯状细胞是诊断性的。通过胃镜可以清楚地看到化生,但必须在显微镜下检查活检标本,以确定细胞是否是胃或结肠。结肠化生通常通过在上皮中发现杯状细胞来鉴定,并且是真正诊断所必需的。
已知许多Barrett食管的组织学模拟物(即,在正常食道粘膜下腺管的过渡上皮中发生的杯状细胞,“假荧光细胞”,其中丰富的中央凹[胃]型粘蛋白模拟酸性粘蛋白真正的杯状细胞)。通过组织检查多个水平评估与粘膜下腺和过渡型上皮的关系可以使病理学家可靠地区分粘膜下腺管的杯状细胞和真正的Barrett食管(专门的柱状化生)。使用组织化学染色剂阿尔新蓝pH 2.5也经常用于区分真正的肠型粘蛋白和它们的组织学模拟物。最近,用CDX-2抗体(特异性用于中肠和后肠肠衍生)的免疫组织化学分析也已被用于鉴定真正的肠型化生细胞。蛋白质AGR2在Barrett食管中升高[16]并且可以用作区分Barrett上皮和正常食管上皮的生物标志物。[17]
Barrett食管中肠上皮化生的存在代表了化生向发育不良和最终腺癌进展的标志物。该因子结合p53,Her2和p16的两种不同的免疫组织化学表达导致两种不同的遗传途径可能发展为Barrett食管的发育不良[18]。肠道化生细胞也可能是CK 7 + / CK20 - 阳性[19]。
上皮发育不良
在对Barrett食管进行初步诊断后,受影响的人接受年度监测,以发现表明癌症进展风险较高的变化:上皮发育不良(或“上皮内瘤变”)的发展。[20]在所有化生性病变中,约8%与不典型增生有关。特别是最近的一项研究表明,发育不良病变主要位于食管后壁[21]。
在病理学家的发育异常评估中可以看到相当大的变异性。最近,胃肠病学和胃肠病理学会建议,在对患者进行最终治疗之前,至少有两名受过奖学金训练的胃肠病学家会证实Barrett的高度异型增生症的诊断。[22]为了获得更高的准确性和可重复性,还建议遵循国际分类系统作为胃肠道上皮瘤形成的“维也纳分类”(2000)。[23]
管理
很多患有Barrett食管的人都没有发育异常。医学协会建议,如果患者患有Barrett食管,并且过去两次内镜检查和活检检查确认没有发育不良,那么患者不应该在三年内进行另一次内镜检查。[24] [25] [26]
通常建议对Barrett食管患者进行内镜监测,但很少有直接证据支持这种做法。[1]高度异型增生的治疗选择包括手术切除食管(食管切除术)或内镜治疗,如内镜下粘膜切除或消融(破坏)。[1]
美国50岁以上的高加索男性患有恶性肿瘤的风险最高,症状超过五年。目前的建议包括常规内窥镜检查和活组织检查(寻找发育异常的变化)。虽然过去医生采取了观察等待的方法,但新发表的研究支持考虑对Barrett食管进行干预。基于气囊的射频消融由Ganz,Stern和Zelickson于1999年发明,是治疗Barrett食管和发育不良的一种新的治疗方式,并且已成为众多已发表的临床试验的主题。[27] [28] [29] ] [30]研究结果表明射频消融治疗Barrett食管完全清除和发育不良的疗效达到90%或更高,耐久性长达5年,安全性良好[27] [28] [29] [30]。
质子泵抑制剂药物和抗反流手术尚未被证实可以预防食道癌。激光治疗用于严重的不典型增生,而明显的恶性肿瘤可能需要手术,放射治疗或全身化疗。最近的一项为期五年的随机对照试验表明,与单独使用质子泵抑制剂相比,使用光敏素进行光动力疗法在统计学上更有效地消除发育不良的生长区域。[31]
目前还没有可靠的方法来确定哪些Barrett食管患者会继续发展食道癌,尽管最近的一项研究发现三种不同的遗传异常的检测与六年内发生癌症的几率高达79%相关。 [32]
内镜下粘膜切除术也被评估为一种管理技术。[33]此外,一种称为Nissen胃底折叠术的手术可以减少酸从胃进入食道的反流。[34]
在各种研究中,非甾体类抗炎药(NSAIDS),如阿司匹林,已经证明可以预防Barrett食管患者的食管癌[35] [36]。 然而,这些研究中没有一项是随机,安慰剂对照试验,被认为是评估医学干预的金标准。 此外,目前还不知道用于预防癌症的最佳NSAID剂量。
预测
Barrettʼs cancer adenocarcinoma(poor;signet-ringcell)
巴雷特的癌症
腺癌(不良;印戒细胞)
巴雷特的食道是一种恶变前的病症。其恶性后遗症,食管胃交界性腺癌,死亡率超过85%。[37]据估计,患有Barrett食管的人患食管腺癌的风险为每1000人年6-7人[38] [39],然而2011年发表的一项来自丹麦的11,028名患者的队列研究显示,发病率仅为1.2每1000人年(发育不良患者为每1000人年5.1人,无发育不良患者为每1000人年1.0人)。[40]
与普通人群相比,Barret食管患者食管腺癌的相对风险约为10。[41]大多数食管癌患者存活不到一年。[42]
流行病学
高加索男性在美国的发病率是白人女性的8倍,是非裔美国男性的5倍。总体而言,Barrett食管的男女比例为10:1。[43]一些研究估计,在两个欧洲人群中,Barrett食管在一般人群中的患病率为1.3%至1.6%(意大利[44]和瑞典[45]),韩国人群为3.6%[46]。
历史
1975年与腺癌进一步联系。[47]
参考:
Shaheen NJ, Richter JE (March 2009). "Barrett oesophagus". Lancet. 373 (9666): 850–61. doi:10.1016/S0140-6736(09)60487-6. PMID 19269522.
Koppert LB, Wijnhoven BP, van Dekken H, Tilanus HW, Dinjens WN (2005). "The molecular biology of esophageal adenocarcinoma". J Surg Oncol. 92 (3): 169–90. doi:10.1002/jso.20359. PMID 16299787.
Stein HJ, Siewert JR (1993). "Barrett's esophagus: pathogenesis, epidemiology, functional abnormalities, malignant degeneration, and surgical management". Dysphagia. 8 (3): 276–88. doi:10.1007/BF01354551. PMID 8359051.
Barrett NR (October 1950). "Chronic peptic ulcer of the oesophagus and 'oesophagitis'". Br J Surg. 38 (150): 175–82. doi:10.1002/bjs.18003815005. PMID 14791960.
DeMeester T (March 2000). "Columnar Mucosa and Intestinal Metaplasia of the Esophagus: Fifty Years of Controversy". Annals of Surgery. 231 (3): 303–21. PMID 10714623.
Allison PR, Johnstone AS (June 1953). "The oesophagus lined with gastric mucous membrane". Thorax. 8: 87–101. doi:10.1111/j.1440-1746.2008.05386.x. PMC 1019247 Freely accessible. PMID 13077502.
Bani-Hani KE, and Bani-Hani BK (2008). "Columnar-lined esophagus: Time to drop the eponym of "Barrett": Historical review". Journal of Gastroenterology and Hepatology. 23 (5): 707–15. doi:10.1111/j.1440-1746.2008.05386.x.
Edelstein ZR, Farrow DC, Bronner MP, Rosen SN, Vaughan TL (August 2007). "Central adiposity and risk of Barrett esophagus". Gastroenterology. 133 (2): 403–11. doi:10.1053/j.gastro.2007.05.026. PMID 17681161.
Reid BJ, Li X, Galipeau PC, Vaughan TL (February 2010). "Barrett oesophagus and oesophageal adenocarcinoma: time for a new synthesis". Nature Reviews Cancer. 10 (2): 87–101. doi:10.1038/nrc2773. PMC 2879265 Freely accessible. PMID 20094044.
Gong L, Debruyne PR, Witek M, Nielsen K, Snook A, Lin JE, Bombonati A, Palazzo J, Schulz S, Waldman SA (2009). "Bile acids initiate lineage-addicted gastroesophageal tumorigenesis by suppressing the EGF receptor-AKT axis". Clin Transl Sci. 2 (4): 286–93. doi:10.1111/j.1752-8062.2009.00131.x. PMID 20443907.
Debruyne PR, Witek M, Gong L, Birbe R, Chervoneva I, Jin T, Domon-Cell C, Palazzo JP, Freund JN, Li P, Pitari GM, Schulz S, Waldman SA (April 2006). "Bile acids induce ectopic expression of intestinal guanylyl cyclase C through nuclear factor-kappaB and Cdx2 in human esophageal cells". Gastroenterology. 130 (4): 1191–206. doi:10.1053/j.gastro.2005.12.032. PMID 16618413.
"Bulimia nervosa complicated by Barrett's esophagus and esophageal cancer". Giejournal.org. Retrieved 28 July 2018.
"Bulimia and cancer - what you need to know - Bulimia Help". Bulimiahelp.org. Retrieved 28 July 2018.
Fléjou JF (2005). "Barrett's oesophagus: from metaplasia to dysplasia and cancer". Gut. 54 Suppl 1: i6–12. doi:10.1136/gut.2004.041525. PMC 1867794 Freely accessible. PMID 15711008.
Bennett, C; Moayyedi, P; Corley, DA; DeCaestecker, J; Falck-Ytter, Y; Falk, G; Vakil, N; Sanders, S; Vieth, M; Inadomi, J; Aldulaimi, D; Ho, KY; Odze, R; Meltzer, SJ; Quigley, E; Gittens, S; Watson, P; Zaninotto, G; Iyer, PG; Alexandre, L; Ang, Y; Callaghan, J; Harrison, R; Singh, R; Bhandari, P; Bisschops, R; Geramizadeh, B; Kaye, P; Krishnadath, S; Fennerty, MB; Manner, H; Nason, KS; Pech, O; Konda, V; Ragunath, K; Rahman, I; Romero, Y; Sampliner, R; Siersema, PD; Tack, J; Tham, TC; Trudgill, N; Weinberg, DS; Wang, J; Wang, K; Wong, JY; Attwood, S; Malfertheiner, P; MacDonald, D; Barr, H; Ferguson, MK; Jankowski, J; BOB CAT, Consortium (May 2015). "BOB CAT: A Large-Scale Review and Delphi Consensus for Management of Barrett's Esophagus With No Dysplasia, Indefinite for, or Low-Grade Dysplasia". The American Journal of Gastroenterology. 110 (5): 662–82; quiz 683. doi:10.1038/ajg.2015.55. PMC 4436697 Freely accessible. PMID 25869390.
Pohler E, Craig AL, Cotton J, Lawrie L, Dillon JF, Ross P, Kernohan N, Hupp TR (2004). "The Barrett's Antigen Anterior Gradient-2 Silences the p53 Transcriptional Response to DNA Damage". Molecular & Cellular Proteomics. 3 (6): 534–547. doi:10.1074/mcp.M300089-MCP200. PMID 14967811.
Murray E, McKenna EO, Burch LR, Dillon J, Langridge-Smith P, Kolch W, Pitt A, Hupp TR (2007). "Microarray-formatted clinical biomarker assay development using peptide aptamers to anterior gradient-2". Biochemistry. 46 (48): 13742–51. doi:10.1021/bi7008739. PMID 17994709.
Salemme, M; Villanacci, V; Cengia, G; Cestari, R; Missale, G; Bassotti, G (2016). "Intestinal metaplasia in Barrett's oesophagus: An essential factor to predict the risk of dysplasia and cancer development". Digestive and Liver Disease. 48 (2): 144–147. doi:10.1016/j.dld.2015.10.021.
Çoban, Ş; Örmeci, N.; Savaş, B.; Ekiz, F.; Ensari, A.; Kuzu, I.; Palabıyıkoğlu, M. (2013). "Evaluation of Barrett's esophagus with CK7, CK20, p53, Ki67, and COX2 expressions using chromoendoscopical examination". Diseases of the Esophagus: Official Journal of the International Society for Diseases of the Esophagus. 26 (2): 189–196. doi:10.1111/j.1442-2050.2012.01352.x. ISSN 1442-2050. PMID 22591041.
Odze RD (2006). "Diagnosis and grading of dysplasia in Barrett's oesophagus". Journal of Clinical Pathology. 59 (10): 1029–38. doi:10.1136/jcp.2005.035337. PMC 1861756 Freely accessible. PMID 17021130.
Bibbò S, Ianiro G, Ricci R, Arciuolo D, Petruzziello L, Spada C, Larghi A, Riccioni ME, Gasbarrini A, Costamagna G, Cammarota G.
Barrett's oesophagus and associated dysplasia are not equally distributed within the esophageal circumference.Dig Liver Dis. 2016 Sep;48(9):1043-7. doi: 10.1016/j.dld.2016.06.020.
Fléjou JF (2005). "Barrett's oesophagus: From metaplasia to dysplasia and cancer". Gut. 54 Suppl 1: i6–12. doi:10.1136/gut.2004.041525. PMC 1867794 Freely accessible. PMID 15711008.
Schlemper RJ, Riddell RH, Kato Y, Borchard F, Cooper HS, Dawsey SM, Dixon MF, Fenoglio-Preiser CM, Fléjou JF, Geboes K, Hattori T, Hirota T, Itabashi M, Iwafuchi M, Iwashita A, Kim YI, Kirchner T, Klimpfinger M, Koike M, Lauwers GY, Lewin KJ, Oberhuber G, Offner F, Price AB, Rubio CA, Shimizu M, Shimoda T, Sipponen P, Solcia E, Stolte M, Watanabe H, Yamabe H (2000). "The Vienna classification of gastrointestinal epithelial neoplasia". Gut. 47 (2): 251–55. doi:10.1136/gut.47.2.251. PMC 1728018 Freely accessible. PMID 10896917.
American Gastroenterological Association, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, American Gastroenterological Association, archived from the original (PDF) on August 9, 2012, retrieved August 17, 2012
Spechler SJ, Sharma P, Souza RF, Inadomi JM, Shaheen NJ (2011). "American Gastroenterological Association Medical Position Statement on the Management of Barrett's Esophagus". Gastroenterology. 140 (3): 1084–1091. doi:10.1053/j.gastro.2011.01.030. PMID 21376940.
Wang KK, Sampliner RE (2008). "Updated Guidelines 2008 for the Diagnosis, Surveillance and Therapy of Barrett's Esophagus". The American Journal of Gastroenterology. 103 (3): 788–97. doi:10.1111/j.1572-0241.2008.01835.x. PMID 18341497.
Fleischer DE, Overholt BF, Sharma VK, Reymunde A, Kimmey MB, Chuttani R, Chang KJ, Muthasamy R, Lightdale CJ, Santiago N, Pleskow DK, Dean PJ, Wang KK (2010). "Endoscopic radiofrequency ablation for Barrett's esophagus: 5-year outcomes from a prospective multicenter trial". Endoscopy. 42 (10): 781–89. doi:10.1055/s-0030-1255779. PMID 20857372.
Shaheen NJ, Sharma P, Overholt BF, Wolfsen HC, Sampliner RE, Wang KK, Galanko JA, Bronner MP, Goldblum JR, Bennett AE, Jobe BA, Eisen GM, Fennerty MB, Hunter JG, Fleischer DE, Sharma VK, Hawes RH, Hoffman BJ, Rothstein RI, Gordon SR, Mashimo H, Chang KJ, Muthusamy VR, Edmundowicz SA, Spechler SJ, Siddiqui AA, Souza RF, Infantolino A, Falk GW, Kimmey MB, Madanick RD, Chak A, Lightdale CJ (2009). "Radiofrequency Ablation in Barrett's Esophagus with Dysplasia". New England Journal of Medicine. 360 (22): 2277–88. doi:10.1056/NEJMoa0808145. PMID 19474425.
Shaheen NJ, Overholt BF, Sampliner RE, Wolfsen HC, Wang KK, Fleischer DE, Sharma VK, Eisen GM, Fennerty MB, Hunter JG, Bronner MP, Goldblum JR, Bennett AE, Mashimo H, Rothstein RI, Gordon SR, Edmundowicz SA, Madanick RD, Peery AF, Muthusamy VR, Chang KJ, Kimmey MB, Spechler SJ, Siddiqui AA, Souza RF, Infantolino A, Dumot JA, Falk GW, Galanko JA, Jobe BA, Hawes RH, Hoffman BJ, Sharma P, Chak A, Lightdale CJ (2011). "Durability of Ablation in Barrett's Esophagus with Dysplasia". Gastroenterology. 141 (2): 460–68. doi:10.1053/j.gastro.2011.04.061. PMC 3152658 Freely accessible. PMID 21679712.
van Vilsteren FG, Pouw RE, Seewald S, Alvarez Herrero L, Sondermeijer CM, Visser M, Ten Kate FJ, Yu Kim Teng KC, Soehendra N, Rösch T, Weusten BL, Bergman JJ (June 2011). "Stepwise radical endoscopic resection versus radiofrequency ablation for Barrett's oesophagus with high-grade dysplasia or early cancer: a multicentre randomised trial". Gut. 60 (6): 765–73. doi:10.1136/gut.2010.229310. PMID 21209124.
Overholt BF, Wang KK, Burdick JS, Lightdale CJ, Kimmey M, Nava HR, Sivak MV, Nishioka N, Barr H, Marcon N, Pedrosa M, Bronner MP, Grace M, Depot M (2007). "Five-year efficacy and safety of photodynamic therapy with Photofrin in Barrett high-grade dysplasia". Gastrointestinal endoscopy. 66 (3): 460–68. doi:10.1016/j.gie.2006.12.037. PMID 17643436.
Galipeau PC, Li X, Blount PL, Maley CC, Sanchez CA, Odze RD, Ayub K, Rabinovitch PS, Vaughan TL, Reid BJ (2007). "NSAIDs modulate CDKN2A, TP53, and DNA content risk for progression to esophageal adenocarcinoma". PLoS Medicine. 4 (2): e67. doi:10.1371/journal.pmed.0040067. PMC 1808095 Freely accessible. PMID 17326708.
Reshamwala PA, Darwin PE (2006). "Endoscopic management of early gastric cancer". Current Opinion in Gastroenterology. 22 (5): 541–5. doi:10.1097/01.mog.0000239870.04457.80. PMID 16891887.
Abbas AE, Deschamps C, Cassivi SD, Allen MS, Nichols FC, Miller DL, Pairolero PC (2004). "The role of laparoscopic fundoplication in Barrett's esophagus". Annals of Thoracic Surgery. 77 (2): 393–96. doi:10.1016/S0003-4975(03)01352-3. PMID 14759403.
Corley DA, Kerlikowske K, Verma R, Buffler P (2003). "Protective association of aspirin/NSAIDs and esophageal cancer: a systematic review and meta-analysis". Gastroenterology. 124 (1): 47–56. doi:10.1053/gast.2003.50008. PMID 12512029.
Vaughan TL, Dong LM, Blount PL, Ayub K, Odze RD, Sanchez CA, Rabinovitch PS, Reid BJ (2005). "Non-steroidal anti-inflammatory drugs and risk of neoplastic progression in Barrett's oesophagus: a prospective study". Lancet Oncol. 6 (12): 945–52. doi:10.1016/S1470-2045(05)70431-9. PMID 16321762.
Holmes RS, Vaughan TL (January 2007). "Epidemiology and pathogenesis of esophageal cancer". Semin Radiat Oncol. 17 (1): 2–9. doi:10.1016/j.semradonc.2006.09.003. PMID 17185192.
Thomas T, Abrams KR, De Caestecker JS, Robinson RJ (December 2007). "Meta analysis: Cancer risk in Barrett's oesophagus". Aliment. Pharmacol. Ther. 26 (11–12): 1465–77. doi:10.1111/j.1365-2036.2007.03528.x. PMID 17900269.
Yousef F, Cardwell C, Cantwell MM, Galway K, Johnston BT, Murray L (August 2008). "The incidence of esophageal cancer and high-grade dysplasia in Barrett esophagus: a systematic review and meta-analysis". Am. J. Epidemiol. 168 (3): 237–49. doi:10.1093/aje/kwn121. PMID 18550563.
Hvid-Jensen F; et al. (2011). "Incidence of adenocarcinoma among patients with Barrett's esophagus". N Engl J Med. 365: 1375–83. doi:10.1056/NEJMoa1103042. PMID 21995385.
Hvid-Jensen F, Pedersen L, Drewes AM, Sørensen HT, Funch-Jensen P (2011). "Incidence of adenocarcinoma among patients with Barrett's esophagus". N. Engl. J. Med. 365 (15): 1375–83. doi:10.1056/NEJMoa1103042. PMID 21995385.
Polednak AP (May 2003). "Trends in survival for both histologic types of esophageal cancer in US surveillance, epidemiology and end results areas". Int. J. Cancer. 105 (1): 98–100. doi:10.1002/ijc.11029. PMID 12672037.
Zajac, P; Holbrook, A; Super, ME; Vogt, M (March–April 2013). "An overview: Current clinical guidelines for the evaluation, diagnosis, treatment, and management of dyspepsia". Osteopathic Family Physician. 5 (2): 79–85. doi:10.1016/j.osfp.2012.10.005.
Zagari RM, Fuccio L, Wallander MA, Johansson S, Fiocca R, Casanova S, Farahmand BY, Winchester CC, Roda E, Bazzoli F (October 2008). "Gastro-oesophageal reflux symptoms, oesophagitis and Barrett's oesophagus in the general population: the Loiano-Monghidoro study". Gut. 57 (10): 1354–9. doi:10.1136/gut.2007.145177. PMID 18424568.
Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, Vieth M, Stolte M, Talley NJ, Agréus L (December 2005). "Prevalence of Barrett esophagus in the general population: an endoscopic study". Gastroenterology. 129 (6): 1825–31. doi:10.1053/j.gastro.2005.08.053. PMID 16344051.
Kim JY, Kim YS, Jung MK, Park JJ, Kang DH, Kim JS, Song CW, Lee SW, Bak YT (April 2005). "Prevalence of Barrett's esophagus in Korea". J. Gastroenterol. Hepatol. 20 (4): 633–36. doi:10.1111/j.1440-1746.2005.03749.x. PMID 15836715.
Naef AP, Savary M, Ozzello L (November 1975). "Columnar-lined lower esophagus: an acquired lesion with malignant predisposition. Report on 140 cases of Barrett esophagus with 12 adenocarcinomas". J. Thorac. Cardiovasc. Surg. 70 (5): 826–35. PMID 1186274. |